Addressing Fallen Arches
Overview

he belly isn't the only part of your body subject to middle-age spread. As we get older, the years of walking and standing can cause feet to spread and flatten out as ligaments that support the arch lose their holding power. The result: the condition known as fallen arches, or flat feet. "Keep in mind that we're talking about 26 bones in the foot that are supported by a series of ligaments, muscle tendons and other connective tissue," says Glenn Gastwirth, D.P.M., deputy executive director of the American Podiatric Medicine Association in Bethesda, Maryland. "Over a period of time, the ligaments stretch out or 'give' under the pressure of your weight-especially if you're overweight. So what usually happens is you go shopping for new shoes one day and suddenly realize that you now need a size 8 when you've always worn a size 6. You may think your foot has grown, but what really happens is that the foot has spread out, both in width and length."
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Diagnosis of flat feet or fallen arches can be made by your health practitioner and is based on the following. Clinical assessment involving visual gait assessment, as well as biomechanical assessment. A detailed family and medical history. A pain history assessment determining the location of painful symptoms. Physical palpation of the feet and painful areas. Imaging such as MRI or x-ray can be used by your practitioner to assist in the diagnosis.
pes cavus
Non Surgical Treatment
Treatment of flat feet may be appropriate if there is associated foot or lower leg pain, or if the condition affects the knees or the lower back. Treatment may include using Orthoses such as an arch support, foot gymnastics or other exercises as recommended by a podiatrist/orthotist or physical therapist. In cases of severe flat feet, orthoses should be used through a gradual process to lessen discomfort. Over several weeks, slightly more material is added to the orthosis to raise the arch. These small changes allow the foot structure to adjust gradually, as well as giving the patient time to acclimatise to the sensation of wearing orthoses. Once prescribed, orthoses are generally worn for the rest of the patient's life. In some cases, surgery can provide lasting relief, and even create an arch where none existed before; it should be considered a last resort, as it is usually very time consuming and costly.
Surgical Treatment
Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths, also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.

he belly isn't the only part of your body subject to middle-age spread. As we get older, the years of walking and standing can cause feet to spread and flatten out as ligaments that support the arch lose their holding power. The result: the condition known as fallen arches, or flat feet. "Keep in mind that we're talking about 26 bones in the foot that are supported by a series of ligaments, muscle tendons and other connective tissue," says Glenn Gastwirth, D.P.M., deputy executive director of the American Podiatric Medicine Association in Bethesda, Maryland. "Over a period of time, the ligaments stretch out or 'give' under the pressure of your weight-especially if you're overweight. So what usually happens is you go shopping for new shoes one day and suddenly realize that you now need a size 8 when you've always worn a size 6. You may think your foot has grown, but what really happens is that the foot has spread out, both in width and length."
Causes
Most cases of flatfeet are simply the result of normal development. When that is not the case, the condition can be caused by a number of factors, including the following, Age, disease, injury, obesity or being overweight, physical abnormality, pregnancy. Flattened arches in adults may result from the stresses of aging, weight gain, and the temporary increase in elastin (protein in connective tissue) due to pregnancy. In some cases, flatfeet are caused by a physical abnormality, such as tarsal coalition (two or more bones in the foot that have grown together) or accessory navicular (an extra bone along the side of the foot). The effects of diseases such as diabetes and rheumatoid arthritis can lead to flatfeet. An injury (e.g., bone fracture, dislocation, sprain or tear in any of the tendons and ligaments in the foot and leg) also can cause flatfeet.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms below. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Diagnosis of flat feet or fallen arches can be made by your health practitioner and is based on the following. Clinical assessment involving visual gait assessment, as well as biomechanical assessment. A detailed family and medical history. A pain history assessment determining the location of painful symptoms. Physical palpation of the feet and painful areas. Imaging such as MRI or x-ray can be used by your practitioner to assist in the diagnosis.
pes cavus
Non Surgical Treatment
Treatment of flat feet may be appropriate if there is associated foot or lower leg pain, or if the condition affects the knees or the lower back. Treatment may include using Orthoses such as an arch support, foot gymnastics or other exercises as recommended by a podiatrist/orthotist or physical therapist. In cases of severe flat feet, orthoses should be used through a gradual process to lessen discomfort. Over several weeks, slightly more material is added to the orthosis to raise the arch. These small changes allow the foot structure to adjust gradually, as well as giving the patient time to acclimatise to the sensation of wearing orthoses. Once prescribed, orthoses are generally worn for the rest of the patient's life. In some cases, surgery can provide lasting relief, and even create an arch where none existed before; it should be considered a last resort, as it is usually very time consuming and costly.
Surgical Treatment
Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths, also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Leg Length Discrepancy Gait Deviations
Overview
Children of many ages can have legs of unequal lengths. The medical diagnosis for this condition is called leg length discrepancy. The difference in length can be as small as one centimeter and as large as six centimeters or more. The greater the discrepancy, the more your child will have difficulty walking and maintaining proper posture. Significant differences in leg length can also cause functional scoliosis and problems with other parts of the legs and lower body. This makes leg length discrepancy treatment very important in order to maintain proper health and function of the child. The greater the difference in leg length, the higher the likelihood of necessary treatment.
Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
The object of treatment for leg length discrepancy is to level the pelvis and equalize the length of the two limbs. Inequalities of 2-2.5 centimeters can be handled with the following. Heel lifts/ adjustable heel lifts can be used inside a shoe where shoes have a full heel counter. Heel lifts may be added to the heel on the outside of the shoe along with an internal heel lift. Full platforms along the forefoot and rearfoot area of a shoe can be added. There are many different adjustable heel lifts available on the market. For treatment of a leg length discrepancy, consult your physician. They may refer you to a Physiotherapist or Chiropractor for determination of the type of LLD. A Certified Pedorthist (Canada) will treat a structural leg length discrepancy with a heel lift or in larger discrepancies a footwear modification.

how can i increase my height after 18?
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
Children of many ages can have legs of unequal lengths. The medical diagnosis for this condition is called leg length discrepancy. The difference in length can be as small as one centimeter and as large as six centimeters or more. The greater the discrepancy, the more your child will have difficulty walking and maintaining proper posture. Significant differences in leg length can also cause functional scoliosis and problems with other parts of the legs and lower body. This makes leg length discrepancy treatment very important in order to maintain proper health and function of the child. The greater the difference in leg length, the higher the likelihood of necessary treatment.

Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
A doctor will generally take a detailed medical history of both the patient and family, including asking about recent injuries or illnesses. He or she will carefully examine the patient, observing how he or she moves and stands. If necessary, an orthopedic surgeon will order X-ray, bone age determinations and computed tomography (CT) scans or magnetic resonance imaging (MRI).
Non Surgical Treatment
The object of treatment for leg length discrepancy is to level the pelvis and equalize the length of the two limbs. Inequalities of 2-2.5 centimeters can be handled with the following. Heel lifts/ adjustable heel lifts can be used inside a shoe where shoes have a full heel counter. Heel lifts may be added to the heel on the outside of the shoe along with an internal heel lift. Full platforms along the forefoot and rearfoot area of a shoe can be added. There are many different adjustable heel lifts available on the market. For treatment of a leg length discrepancy, consult your physician. They may refer you to a Physiotherapist or Chiropractor for determination of the type of LLD. A Certified Pedorthist (Canada) will treat a structural leg length discrepancy with a heel lift or in larger discrepancies a footwear modification.

how can i increase my height after 18?
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
All The Things You Ought To Know About
Overview

Heel pain may develop when you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues. A sore heel will usually get better on its own if you give it enough rest. Unfortunately, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it and this can lead to chronic pain. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel. Pain beneath the Heel. If it hurts under your heel, you may have one or more conditions that cause inflammation of the tissues on the bottom of your foot. Stone bruise. By stepping on a hard object, you can bruise the fat pad on the bottom side of your heel. It may or may not look discoloured. With rest, the pain subsides gradually.
Causes
Heel pain can have many causes. If your heel hurts, see your primary care doctor or orthopaedic foot and ankle specialist right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you've had it. Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis. In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non Surgical Treatment
Initial treatment should consist of an ice pack. Some runners prefer to use a wet towel that has been in the fridge. We recommend you use commercially available ice packs for focused pain released. An anti-inflammatory such as Ibuprofen will help to reduce the swelling. Please note this should be taken with meals and never before running. As with all soft tissue injuries, you may have to re-examine your training regime. A reduction or even a total break form running may be necessary. . Examine your running shoes, making sure the shoes do not bend excessively near the middle of the foot and at the ball of the foot. Sports shoes with built in insoles can be beneficial, however we recommend you replace existing insoles with specific sports orthotics/ insoles. Silicone heel cups, leather heel pads and contrasting cold and hot therapy can all help to speed up the healing process. The plantar fascia stretch will help to prevent the injury from occurring again. Please note that this stretch should not be done while the heel is inflamed and should only be attempted once you?re a feeling minimal or no pain from your heel.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
heel cushion silicone
Prevention

A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don?t underestimate your body's need for rest and good nutrition. If obese, lose weight.

Heel pain may develop when you pound your feet on hard surfaces playing sports or wear shoes that irritate sensitive tissues. A sore heel will usually get better on its own if you give it enough rest. Unfortunately, many people try to ignore the early signs of heel pain and keep on doing the activities that caused it and this can lead to chronic pain. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel. Pain beneath the Heel. If it hurts under your heel, you may have one or more conditions that cause inflammation of the tissues on the bottom of your foot. Stone bruise. By stepping on a hard object, you can bruise the fat pad on the bottom side of your heel. It may or may not look discoloured. With rest, the pain subsides gradually.
Causes
Heel pain can have many causes. If your heel hurts, see your primary care doctor or orthopaedic foot and ankle specialist right away to determine why and get treatment. Tell him or her exactly where you have pain and how long you've had it. Your doctor will examine your heel, looking and feeling for signs of tenderness and swelling. You may be asked to walk, stand on one foot or do other physical tests that help your doctor pinpoint the cause of your sore heel. Conditions that cause heel pain generally fall into two main categories: pain beneath the heel and pain behind the heel.
Symptoms
See your doctor immediately if you have Severe pain and swelling near your heel. Inability to bend your foot downward, rise on your toes or walk normally. Heel pain with fever, numbness or tingling in your heel. Severe heel pain immediately after an injury. Schedule an office visit if you have. Heel pain that continues when you're not walking or standing. Heel pain that lasts more than a few weeks, even after you've tried rest, ice and other home treatments.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis. In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non Surgical Treatment
Initial treatment should consist of an ice pack. Some runners prefer to use a wet towel that has been in the fridge. We recommend you use commercially available ice packs for focused pain released. An anti-inflammatory such as Ibuprofen will help to reduce the swelling. Please note this should be taken with meals and never before running. As with all soft tissue injuries, you may have to re-examine your training regime. A reduction or even a total break form running may be necessary. . Examine your running shoes, making sure the shoes do not bend excessively near the middle of the foot and at the ball of the foot. Sports shoes with built in insoles can be beneficial, however we recommend you replace existing insoles with specific sports orthotics/ insoles. Silicone heel cups, leather heel pads and contrasting cold and hot therapy can all help to speed up the healing process. The plantar fascia stretch will help to prevent the injury from occurring again. Please note that this stretch should not be done while the heel is inflamed and should only be attempted once you?re a feeling minimal or no pain from your heel.
Surgical Treatment
Although most patients with plantar fasciitis respond to non-surgical treatment, a small percentage of patients may require surgery. If, after several months of non-surgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you. No matter what kind of treatment you undergo for plantar fasciitis, the underlying causes that led to this condition may remain. Therefore, you will need to continue with preventive measures. Wearing supportive shoes, stretching, and using custom orthotic devices are the mainstay of long-term treatment for plantar fasciitis.
heel cushion silicone
Prevention

A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don?t underestimate your body's need for rest and good nutrition. If obese, lose weight.
Mortons Neuroma Remedies
Overview
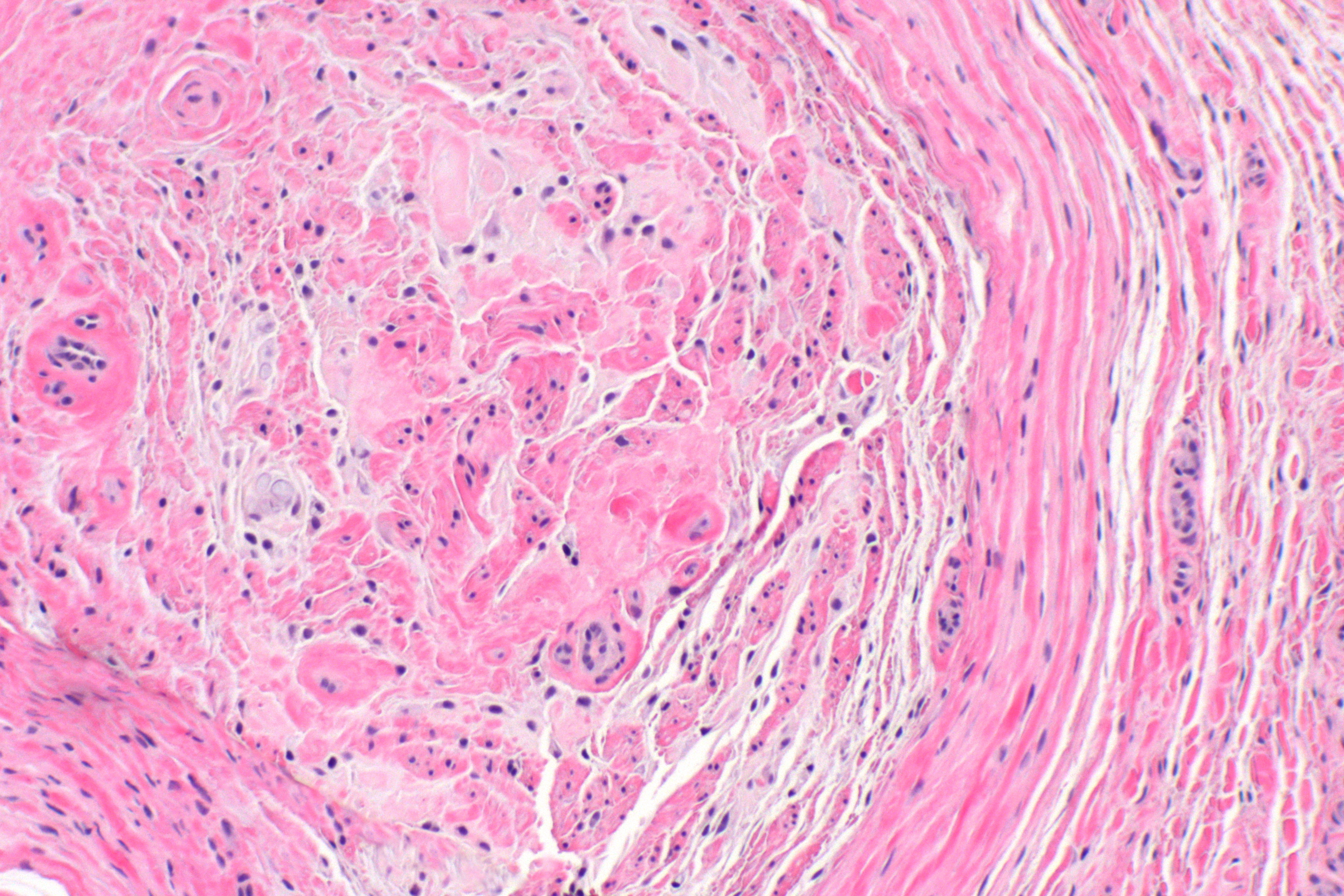 A neuroma develops when a nerve is compressed, injured or pinched, causing swelling and pain. A neuroma in the area between the third and fourth toes, or between the second and third toes, is known as a Morton?s neuroma. Morton?s neuroma causes sharp, burning pain and numbness in the toes and foot. You may feel like you?ve stepped on a tiny hot coal and can?t get rid of it. At the same time, you?ll have the disconcerting experience of not being able to feel your toes. Sometimes the nerve tissue becomes so thickened you can feel or see a lump.
A neuroma develops when a nerve is compressed, injured or pinched, causing swelling and pain. A neuroma in the area between the third and fourth toes, or between the second and third toes, is known as a Morton?s neuroma. Morton?s neuroma causes sharp, burning pain and numbness in the toes and foot. You may feel like you?ve stepped on a tiny hot coal and can?t get rid of it. At the same time, you?ll have the disconcerting experience of not being able to feel your toes. Sometimes the nerve tissue becomes so thickened you can feel or see a lump.
Causes
The exact cause is unknown. Doctors believe the following may play a role in the development of this condition. Wearing tight shoes and high heels. Abnormal positioning of toes. Flat feet. Forefoot problems, including bunions and hammer toes. High foot arches. Morton neuroma is more common in women than in men.
Symptoms
Pain is usually increased by forefoot weight bearing activities (such as running), with narrow-fitting footwear, or with high heeled shoes. It is usually painful to firmly touch the affected region and, in chronic cases, pain and sometimes an audible click, may be heard when squeezing the foot and toes together with the hand. Often a localized area of swelling may be evident at the site of injury.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
Once a diagnosis is obtained, it is essential to begin treatment immediately. Your podiatric physician will advise you on the most effective means. If caught early enough, good foot care, shoes that fit properly, and/or orthoses may eliminate the need for any further intervention. Other conservative measures might include oral non-steroidal anti-inflammatory medication (NSAIDS), physical therapy, ultrasound or other non-invasive measures. If that doesn?t work, your podiatric physician might use injectable steroids, and/or a local anesthetic around the neuroma to reduce inflammation and pain. Many patients report relief after these measures are taken.
Surgical Treatment
Operative treatment of Morton?s neuroma should be entertained only after failure of nonoperative management. Standard operative treatment involves identifying the nerve and cutting (resecting) it proximal to the point where it is irritate/injured. This is usually done through an incision on the top (dorsal) aspect of the foot, although in rare instances, an incision on the sole (plantar) aspect of the foot maybe used. An incision on the sole of the foot works very well, unless an excessive scar forms in which case it can be problematic. Some physicians will attempt to treat Morton?s neuroma by releasing the intermetatarsal ligament and freeing the nerve of local scar tissue. This may also be beneficial.
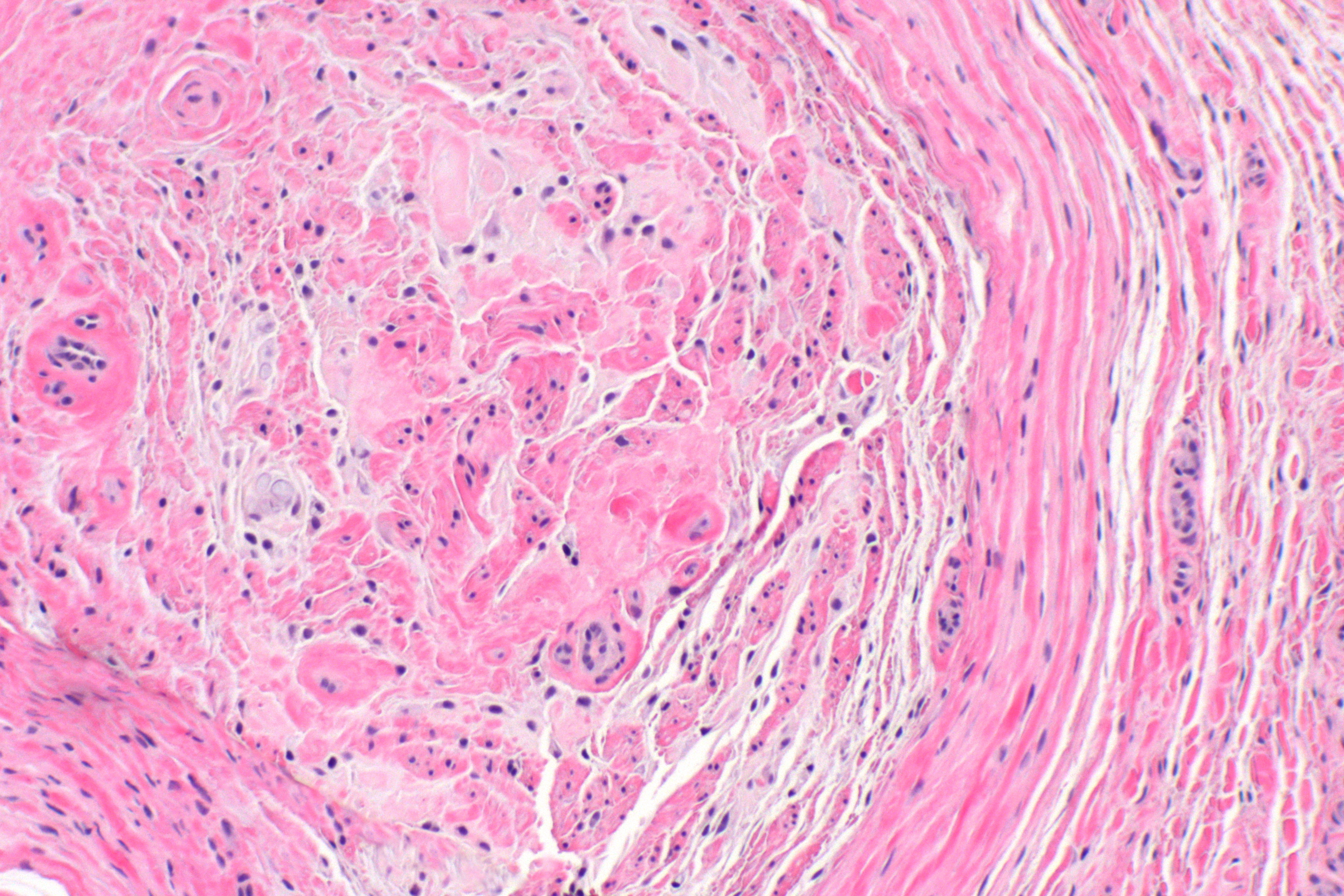 A neuroma develops when a nerve is compressed, injured or pinched, causing swelling and pain. A neuroma in the area between the third and fourth toes, or between the second and third toes, is known as a Morton?s neuroma. Morton?s neuroma causes sharp, burning pain and numbness in the toes and foot. You may feel like you?ve stepped on a tiny hot coal and can?t get rid of it. At the same time, you?ll have the disconcerting experience of not being able to feel your toes. Sometimes the nerve tissue becomes so thickened you can feel or see a lump.
A neuroma develops when a nerve is compressed, injured or pinched, causing swelling and pain. A neuroma in the area between the third and fourth toes, or between the second and third toes, is known as a Morton?s neuroma. Morton?s neuroma causes sharp, burning pain and numbness in the toes and foot. You may feel like you?ve stepped on a tiny hot coal and can?t get rid of it. At the same time, you?ll have the disconcerting experience of not being able to feel your toes. Sometimes the nerve tissue becomes so thickened you can feel or see a lump.Causes
The exact cause is unknown. Doctors believe the following may play a role in the development of this condition. Wearing tight shoes and high heels. Abnormal positioning of toes. Flat feet. Forefoot problems, including bunions and hammer toes. High foot arches. Morton neuroma is more common in women than in men.
Symptoms
Pain is usually increased by forefoot weight bearing activities (such as running), with narrow-fitting footwear, or with high heeled shoes. It is usually painful to firmly touch the affected region and, in chronic cases, pain and sometimes an audible click, may be heard when squeezing the foot and toes together with the hand. Often a localized area of swelling may be evident at the site of injury.
Diagnosis
Your health care provider can usually diagnose this problem by examining your foot. A foot x-ray may be done to rule out bone problems. MRI or high-resolution ultrasound can successfully diagnose Morton's neuroma. Nerve testing (electromyography) cannot diagnose Morton's neuroma, but may be used to rule out conditions that cause similar symptoms. Blood tests may be done to check for inflammation-related conditions, including certain forms of arthritis.
Non Surgical Treatment
Once a diagnosis is obtained, it is essential to begin treatment immediately. Your podiatric physician will advise you on the most effective means. If caught early enough, good foot care, shoes that fit properly, and/or orthoses may eliminate the need for any further intervention. Other conservative measures might include oral non-steroidal anti-inflammatory medication (NSAIDS), physical therapy, ultrasound or other non-invasive measures. If that doesn?t work, your podiatric physician might use injectable steroids, and/or a local anesthetic around the neuroma to reduce inflammation and pain. Many patients report relief after these measures are taken.

Surgical Treatment
Operative treatment of Morton?s neuroma should be entertained only after failure of nonoperative management. Standard operative treatment involves identifying the nerve and cutting (resecting) it proximal to the point where it is irritate/injured. This is usually done through an incision on the top (dorsal) aspect of the foot, although in rare instances, an incision on the sole (plantar) aspect of the foot maybe used. An incision on the sole of the foot works very well, unless an excessive scar forms in which case it can be problematic. Some physicians will attempt to treat Morton?s neuroma by releasing the intermetatarsal ligament and freeing the nerve of local scar tissue. This may also be beneficial.
Shoe Lifts The Industry experts Treatment For Leg Length Difference
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is anatomically shorter than the other. Through developmental phases of aging, the brain picks up on the stride pattern and recognizes some difference. Our bodies typically adapts by dipping one shoulder over to the "short" side. A difference of less than a quarter inch is not grossly irregular, doesn't need Shoe Lifts to compensate and mostly does not have a profound effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this problem is simply fixed, and can eradicate a number of cases of lower back pain.
Treatment for leg length inequality commonly involves Shoe Lifts. Many are low cost, generally costing below twenty dollars, in comparison to a custom orthotic of $200 or higher. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Back ache is easily the most widespread health problem impacting people today. Around 80 million men and women suffer from back pain at some stage in their life. It's a problem that costs companies vast amounts of money each year as a result of lost time and productivity. Innovative and better treatment methods are constantly sought after in the hope of lowering economic impact this issue causes.

Men and women from all corners of the earth experience foot ache as a result of leg length discrepancy. In these cases Shoe Lifts are usually of very helpful. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by countless professional orthopaedic physicians.
In order to support the human body in a healthy and balanced manner, feet have a critical job to play. Despite that, it is often the most overlooked region in the human body. Many people have flat-feet which means there may be unequal force placed on the feet. This causes other body parts including knees, ankles and backs to be affected too. Shoe Lifts guarantee that suitable posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, yet this problem is simply fixed, and can eradicate a number of cases of lower back pain.
Treatment for leg length inequality commonly involves Shoe Lifts. Many are low cost, generally costing below twenty dollars, in comparison to a custom orthotic of $200 or higher. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Back ache is easily the most widespread health problem impacting people today. Around 80 million men and women suffer from back pain at some stage in their life. It's a problem that costs companies vast amounts of money each year as a result of lost time and productivity. Innovative and better treatment methods are constantly sought after in the hope of lowering economic impact this issue causes.

Men and women from all corners of the earth experience foot ache as a result of leg length discrepancy. In these cases Shoe Lifts are usually of very helpful. The lifts are capable of easing any discomfort in the feet. Shoe Lifts are recommended by countless professional orthopaedic physicians.
In order to support the human body in a healthy and balanced manner, feet have a critical job to play. Despite that, it is often the most overlooked region in the human body. Many people have flat-feet which means there may be unequal force placed on the feet. This causes other body parts including knees, ankles and backs to be affected too. Shoe Lifts guarantee that suitable posture and balance are restored.
Best Ways To Treat Calcaneal Spur

Overview
Heel spurs are a common reason for people to visit their podiatrist serving Scottsdale. These small calcium deposits can cause major pain, but treatments are available to relieve your symptoms. Heel spurs grow along the plantar fascia and create a sensation similar to that of a pebble being stuck in your shoe. Your podiatrist will use a physical exam plus X-rays to determine if a heel spur is the cause of your foot pain before beginning treatment. If you do have a heel spur, your podiatrist may recommend a cortisone injection to ease inflammation. Other techniques, such as stretching the calf muscles, treating the heel with ice, and wearing a custom orthotic may also provide relief from the discomfort of a heel spur.
Causes
Heel spurs develop as an abnormal growth in the heel bone due to calcium deposits that form when the plantar fascia pulls away from the heel. This stretching of the plantar fascia is usually the result of over-pronation (flat feet), but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.

Symptoms
Although it may take years to become a problem, once it appears, it may cause considerable suffering. Because of proximity to the tendons, the spur is a source of continuous painful aching. The sensation has been described as "a toothache in the foot." When you place your weight on the heel, the pain can be sufficient to immobilize you.
Diagnosis
Heel spurs and plantar fasciitis is usually diagnosed by your physiotherapist or sports doctor based on your symptoms, history and clinical examination. After confirming your heel spur or plantar fasciitis they will investigate WHY you are likely to be predisposed to heel spurs and develop a treatment plan to decrease your chance of future bouts. X-rays will show calcification or bone within the plantar fascia or at its insertion into the calcaneus. This is known as a calcaneal or heel spur. Ultrasound scans and MRI are used to identify any plantar fasciitis tears, inflammation or calcification. Pathology tests may identify spondyloarthritis, which can cause symptoms similar to plantar fasciitis.
Non Surgical Treatment
Diathermy treatment uses an electrical current to produce heat that sedates the inflamed tissues. The ultrasound device sends sound waves into the heel and sets up a massaging action that stimulates blood circulation. Treatment with a whirlpool bath involves placing the foot directly into the jetting stream. Orthopedic molds and appliances, such as orthotics, are designed by foot specialists for use inside the shoe to eliminate irritation to the heel when the patient stands or walks. When those appliances are used, the spur (in effect) floats on air. At the same time, the body's weight is transferred forward from the tender spot.
Surgical Treatment
Approximately 2% of people with painful heel spurs need surgery, meaning that 98 out of 100 people do well with the non-surgical treatments previously described. However, these treatments can sometimes be rather long and drawn out, and may become considerably expensive. Surgery should be considered when conservative treatment is unable to control and prevent the pain. If the pain goes away for a while, and continues to come back off and on, despite conservative treatments, surgery should be considered. If the pain really never goes away, but reaches a plateau, beyond which it does not improve despite conservative treatments, surgery should be considered. If the pain requires three or more injections of "cortisone" into the heel within a twelve month period, surgery should be considered.
Prevention
If you have not yet developed this condition, you can take steps to protect yourself from it. Most importantly, make it a rule to wear properly fitted footwear. Avoid shoes that have become worn down in the heel, and don't choose shoes that cause you to walk in an abnormal fashion. Maintaining a healthy weight will ensure that undue pressure isn't being put on the ligaments, tendons and bones of your feet. If your job requires a great deal of time on your feet, or if you exercise regularly, be sure to balance periods of activity with periods of rest for your feet.
Will A Calcaneal Spur Hurt?

Overview
A heel spur is a bony projection at the base of the heel bone, as defined by the website webmd.com. Heel spurs are often accompanied by plantar fasciitis, the inflammation of the soft tissues surrounding the spur, and that is what causes the pain in those who suffer from this condition. To cure or remove a heel spur you will need to see a podiatrist; however, there are some natural remedies and exercises that may help.
Causes
Heel spurs develop as an abnormal growth in the heel bone due to calcium deposits that form when the plantar fascia pulls away from the heel. This stretching of the plantar fascia is usually the result of over-pronation (flat feet), but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.

Symptoms
Heel spurs may or may not cause symptoms. Symptoms are usually related to the plantar fasciitis. You may experience significant pain. Your heel pain may be worse in the morning when you first wake up or during certain activities.
Diagnosis
Diagnosis is made using a few different technologies. X-rays are often used first to ensure there is no fracture or tumor in the region. Then ultrasound is used to check the fascia itself to make sure there is no tear and check the level of scar tissue and damage. Neurosensory testing, a non-painful nerve test, can be used to make sure there is not a local nerve problem if the pain is thought to be nerve related. It is important to remember that one can have a very large heel spur and no plantar fasciitis issues or pain at all, or one can have a great deal of pain and virtually no spur at all.
Non Surgical Treatment
There are both conservative and surgical heel spur treatment options. Because the heel pain caused by heel spurs is symptomatic of inflammation, the first step is to ice the area in hopes to reduce the inflammation. The next step is to see our orthopedic specialist to prescribe an appropriate treatment plan. Some conservative treatment options might include Anti-inflammatory medications. Shoe orthotics. Shoe inserts. If conservative treatments are not working, surgery may be required to remove the heel spur. As in all cases of heel pain, it is important to see an orthopedic doctor who specializes in foot and ankle pain.
Surgical Treatment
In some cases, heel spurs are removed by surgery after an X-ray. While the surgery is typically effective, it?s a timely and expensive procedure. Even after surgery, heel spurs can re-form if the patient continues the lifestyle that led to the problem. These reasons are why most people who develop painful heel spurs begin looking for natural remedies for joint and bone pain. Surgery isn?t required to cure a heel spur. In fact, more than 90 percent of people get better with nonsurgical treatments. If nonsurgical methods fail to treat symptoms of heel spurs after 12 months, surgery may be necessary to alleviate pain and restore mobility.
Prevention
You can prevent heel spurs by wearing well-fitting shoes with shock-absorbent soles, rigid shanks, and supportive heel counters; choosing appropriate shoes for each physical activity; warming up and doing stretching exercises before each activity; and pacing yourself during the activities. Avoid wearing shoes with excessive wear on the heels and soles. If you are overweight, losing weight may also help prevent heel spurs.